Coronary ischemia, an overview of ischemic heart disease
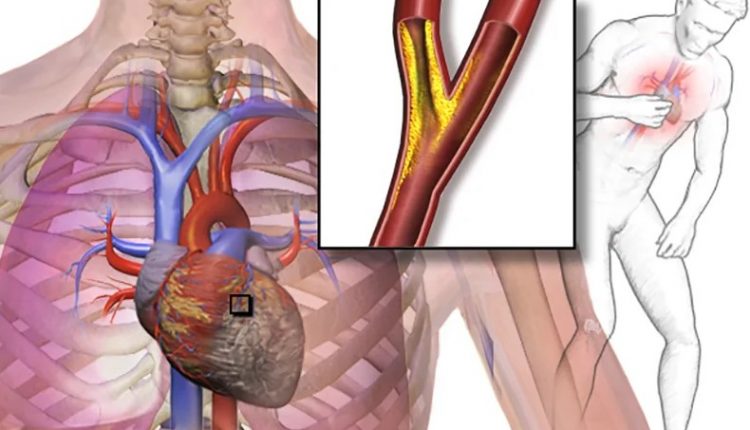
Coronary ischemia, a pathology also known by the medical term of “ischemic heart disease”, involves an important state of suffering of the heart muscle caused – as the term itself suggests – by a reduced supply of oxygenated blood induced, in most cases, by an occlusion of the coronary arteries
The coronary arteries are the main system through which the heart muscle is supplied.
Thanks to these vessels, the blood, oxygenated by the passage in the pulmonary circulation, reaches the heart.
These arteries, due to causes that we will investigate later, can undergo an occlusion, which generates ischemia: a decrease or even an interruption of the blood supply to a specific body district, the heart, in this case.
The tissue affected by ischemia will find itself facing a reduced oxygen supply, a reduced supply of nutrients and the impossibility of eliminating waste substances, as happens physiologically.
This situation will cause severe suffering for the affected tissues, which – if subjected to ischemia for a long time – can also be profoundly compromised in their functionality.
What are the causes and risk factors of coronary ischemia?
Going to investigate the causes of coronary ischemia, we will focus on those that are responsible for the occlusion of the coronary arteries.
This occlusion – known, more generally, by the term coronary artery disease – recognizes its main cause in atherosclerosis.
With atherosclerosis, we indicate the degenerative pathology affecting the vessel wall that leads to an accumulation of cholesterol and other substances in this site.
The affected vessels see their lumen and the elasticity of their walls progressively decrease
The blood, having to pass through a narrower and more rigid channel than normal, increases its pressure, jeopardizing the integrity of the artery itself which, if injured, could favor the formation of thrombi.
Thrombi are a mass of coagulated blood which, traveling inside the blood vessels, can reach the coronary arteries, partially or completely occluding them.
As already explained, occlusion is the main cause of coronary ischemia
Among the risk factors that can lead to the development of coronary ischemia are hypertension (high blood pressure), hypercholesterolemia, elevated triglycerides, advanced age, tobacco smoke, diabetes mellitus, obesity and some inflammatory diseases.
Coronary ischemia: recognize the symptoms
Recognizing the symptoms linked to coronary ischemia may not be simple and immediate.
The symptoms are, in fact, not very specific and very similar to other conditions that can affect the heart muscle.
In any case, one of the first symptoms to be felt by the patient is discomfort or pain in the chest.
In fact, coronary ischemia begins to manifest itself with a sharp pain in the chest that appears suddenly, usually accompanied by a sense of oppression in the same area of the body.
Secondary symptoms of coronary ischemia can be shortness of breath, excessive sweating, sudden pain in the left shoulder and/or arm, feeling tired, fainting, dyspnoea, nausea, sudden anxiety and vomiting.
The severity and duration of coronary ischemia determine whether or not the damage that the tissue undergoes due to lack of oxygen is reversible.
It is estimated that the heart muscle – or a part of it – can withstand a reduction in oxygen and nutrients for a time ranging from 20 to 360 minutes, depending on the amount of blood that the muscle is able to receive by other routes.
After this period of time, the cardiac tissue goes into necrosis, losing its physiological function.
The cells in necrosis are to be considered completely unrecoverable and – in their place – fibrous and inert scar tissue is formed.
Diagnose coronary ischemia
When the symptoms described above are felt and there is a suspicion of coronary ischemia in progress, it is necessary to promptly go to the emergency room to be examined by a specialist.
Here, after the triage, a cardiologist will examine the case, starting with taking a thorough patient history. Investigating your lifestyle, habits and personal and family medical history will help the professional formulate a correct diagnosis.
The medical history will be followed by the request – by the cardiologist – to perform a series of diagnostic tests, including the electrocardiogram, the echocardiogram, the blood tests and, possibly, the coronary angioTAC.
The electrocardiogram is a test that detects and records the electrical activity of the heart and that allows you to view any abnormalities in the beat attributable to an ongoing coronary ischemia.
The echocardiogram is an ultrasound of the heart useful to show any alterations due to ischemia and coronary occlusion.
Blood tests, during a coronary ischemia, are essential to detect the presence of certain substances that are specifically released by the heart muscle when there is a necrosis of its cells.
The coronary angioTAC is a contrast medium examination that allows to study the blood circulation inside the coronary arteries, so as to be able to identify any obstructions present.
Coronary ischemia: the most appropriate therapy
The greater the time that has passed since the onset of coronary ischemia, the more concrete the possibility that the muscle will undergo progressive deterioration, up to necrosis.
Prompt intervention is the best way to try to restore the functionality of the heart muscle and this will only be possible by restoring the correct blood flow in the coronary arteries, so as to once again spray the tissue with oxygen and nutrients.
Drug therapy involves the use of anticoagulant drugs such as heparin or antiplatelet agents such as aspirin to inhibit blood clotting and thin it, thus making it less prone to form further clots.
Thrombolytics can then also be administered to dissolve the thrombus that blocks blood flow in the coronary arteries towards the heart.
If appropriate, beta-blockers, ACE inhibitors and angiotensin II receptor blockers may also be given to try to reduce blood pressure.
However, drug therapy may not be sufficient to resolve the coronary ischemia in progress.
Depending on the clinical condition, the patient may undergo surgery.
A coronary angioplasty with coronary stenting will be performed to widen the blocked coronary arteries, so that blood can flow back to the heart.
This procedure is done by inserting a catheter with a balloon tip that is inflated at the blockage to dilate the coronary artery and restore flow.
Subsequently, with the aid of a guide wire, the stent is inserted and positioned which, once the balloon has deflated, will remain in position preventing the artery from closing again.
Alternatively, coronary bypass surgery can be performed, which is useful for creating a new passageway for blood, an alternative to the one that is occluded.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Ventricular Fibrillation Is One Of The Most Serious Cardiac Arrhythmias: Let’s Find Out About It
Patent Foramen Ovale: Definition, Symptoms, Diagnosis And Consequences
Sinus Tachycardia: What It Is And How To Treat It
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Aorta Surgery: What It Is, When It Is Essential
Abdominal Aortic Aneurysm: Symptoms, Evaluation And Treatment
Spontaneous Coronary Artery Dissection, Which Heart Disease Is Associated With
Coronary Artery Bypass Surgery: What It Is And When To Use It
Do You Have To Face Surgery? Post-Surgery Complications
What Is Aortic Regurgitation? An Overview
Diseases Of The Valves Of The Heart: Aortic Stenosis
Interventricular Septal Defect: What It Is, Causes, Symptoms, Diagnosis, And Treatment
Heart Disease: The Atrial Septal Defect
Interventricular Defect: Classification, Symptoms, Diagnosis And Treatment
Arrhythmias: The Alterations Of The Heart
Identifying Tachycardias: What It Is, What It Causes And How To Intervene On A Tachycardia
Cardiac Rhythm Disturbance Emergencies: The Experience Of US Rescuers
Cardiomyopathies: Definition, Causes, Symptoms, Diagnosis And Treatment
How To Use An AED On A Child And An Infant: The Paediatric Defibrillator
Aortic Valve Surgery: An Overview
Cutaneous Manifestations Of Bacterial Endocarditis: Osler Nodes And Janeway’s Lesions
Bacterial Endocarditis: Prophylaxis In Children And Adults
Infective Endocarditis: Definition, Symptoms, Diagnosis And Treatment
Atrial Flutter: Definition, Causes, Symptoms, Diagnosis And Treatment



