Cysts in the biliary tract: Caroli disease
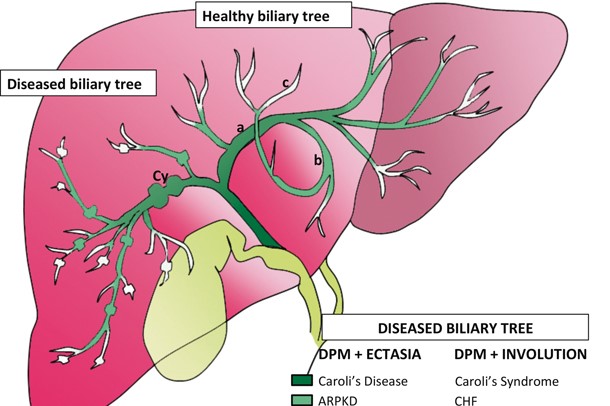
A particular pathology, often considered among the cystic liver diseases, is Caroli disease or Caroli syndrome: it is characterised by cysts communicating with the intrahepatic biliary tract
Caroli’s disease is rare and is due to a congenital malformation of the biliary tract, either isolated or associated with another liver disease, congenital hepatic fibrosis.
In this case, the disease is hereditary and it is possible that a renal malformation, such as polycystic kidney, is also associated.
Caroli syndrome can run asymptomatic for a long time
The first clinical manifestations are fevers: onset with shivering chills, fever peaks reaching 39°C and above, which quickly cease with profuse sweating.
If these febrile outbreaks are not accompanied by jaundice or pain, the relation to a biliary infection is often overlooked.
The appearance, together with fever, of jaundice and pain usually means that stones have formed in the cystic dilatations.
Diagnostics should be based on ultrasound, computed tomography (CT) and magnetic resonance cholangiography and demonstrate the main differential characteristic of these cysts, which is their communication with the intrahepatic biliary tract.
Endoscopic cholangiography should be avoided because it exposes the patient to the risk of biliary infection, which can be very serious in these cases.
The evolution of the syndrome is dominated by the recurrence of febrile seizures that occur with variable frequency and are usually very serious.
The presence of stones in the cystic dilatations causes true biliary colic and can lead to both obstructive jaundice and acute pancreatitis.
When an infection is present, it can evolve unpredictably towards septicaemia and the formation of liver abscesses. Finally, it is recognised that there is a risk of cancer in this disease.
Treatment of Caroli syndrome is solely surgical
But certain interventions should be avoided.
The treatment of Caroli syndrome is the surgical removal of cystic dilatations, but this is possible when the disease only affects a part of the liver.
If, on the other hand, the disease has spread to the whole liver, surgery is not justified even if the only aim is to remove the most diseased part.
The remaining part would still be exposed to new infections and the risk of cancer.
The most logical treatment in disease spreading to the whole liver is transplantation, which may be made difficult in those cases that have already undergone previous surgery.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Acute Liver Failure In Childhood: Liver Malfunction In Children
The Different Types Of Hepatitis: Prevention And Treatment
Acute Hepatitis And Kidney Injury Due To Energy Drink Consuption: Case Report
New York, Mount Sinai Researchers Publish Study On Liver Disease In World Trade Center Rescuers
Acute Hepatitis Cases In Children: Learning About Viral Hepatitis
Hepatic Steatosis: Causes And Treatment Of Fatty Liver
Hepatopathy: Non-Invasive Tests To Assess Liver Disease
Liver: What Is Non-Alcoholic Steatohepatitis
Symptoms And Treatment For Hypothyroidism
Hyperthyroidism: Symptoms And Causes
Surgical Management Of The Failed Airway: A Guide To Precutaneous Cricothyrotomy
Thyroid Cancers: Types, Symptoms, Diagnosis
Benign Tumours Of The Liver: We Discover Angioma, Focal Nodular Hyperplasia, Adenoma And Cysts



