Folie à deux (shared psychotic disorder): causes, symptoms, consequences, diagnosis and treatment
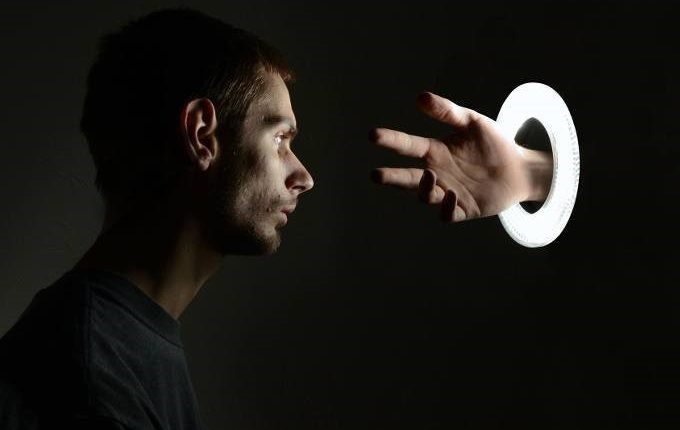
Shared psychotic disorder’, also called Lasègue-Falret syndrome or ‘shared psychosis’ or ‘folie à deux’ (i.e. ‘madness shared by two’) in psychiatry refers to a very rare psychiatric syndrome in which a symptom of psychosis – typically a paranoid or delusional belief – is transmitted from one individual to another
The effect is such that both individuals suffer from the same delusions and/or hallucinations in a synergistic and potentially exponential manner.
In English, the disorder is called “shared psychosis” or “shared delusional disorder” or “Lasègue-Falret syndrome” or “induced delusional disorder” or “shared psychotic disorder”.
Lasègue-Falret syndrome, when shared by more than two people, may be called folie à trois (madness of three), folie à quatre (madness of four), folie à famille (family madness) or even folie à plusieurs (madness of many) depending on the number of people involved.
The madness of many typically occurs in grouped individuals, where one individual (the ‘guru’) convinces the other individuals, who are part of the ‘sect’, of their delusional beliefs.
Generally, affected individuals live in contact or are socially or physically isolated and have little interaction with other people.
Lasègue-Falret syndrome owes its name to the two French psychiatrists who first described it in the 19th century: Charles Lasègue and Jules Falret.
Shared delusional disorder is most commonly found in women with a slightly above average IQ, who are isolated from their family and who have relationships with a dominant person who has delusions.
Most cases also meet the criteria for dependent personality disorder, characterised by a pervasive fear that leads them to need constant reassurance, support and guidance.
More than half of the cases have a relative with a psychological disorder that includes delusions.
The shared psychotic disorder can be of two types, ‘imposée’ and ‘simultanée
Folie imposée (two-imposed madness)
In folie imposée, a dominant person (known as the ‘inducer’, ‘primary’ or ‘principal’) initially creates a delusional thought during a psychotic episode and imposes it on another person or persons (known as the ‘secondary(s)’ or ‘associate(s)’), assuming that the ‘secondary(s)’ subject(s) would not have had the psychotic disorder if they had not interacted with the inducer.
In this case, if the individuals are hospitalised separately, the delusions of the induced person(s) usually disappear without the use of drugs.
Folie simultanée (simultaneous twosome madness)
In folie simultanée two or more persons, who independently suffer from psychosis, influence the content of their respective delusions so that they become the same or very similar.
In this case, if the individuals are hospitalised separately, the delusions of each psychotic individual remain, but tend to become different again.
Causes of shared psychotic disorder
The exact causes of twosome madness are unknown, however, two main risk factors contributing to the development of the disorder are known: intense stress and social isolation.
People who are socially isolated together tend to become dependent on those with whom they are isolated, leading to an inducing influence on those around them.
In fact, people who develop a shared delusional disorder do not have others who can remind them that their ideas are impossible or improbable, so delusions become cemented in the minds of isolated individuals.
It is precisely for this reason that the treatment for delusional disorder requires the affected persons to be separated from one another.
Intense and prolonged psycho-physical stress, especially in connection with shocks and highly traumatic events (e.g. witnessing the violent death of one’s parents) is also a common factor in the development or worsening of various mental illnesses, including insanity in twos.
Most people who develop a shared delusional disorder are genetically predisposed to mental illness, but this predisposition is generally not sufficient to develop a mental disorder: stress can act as a trigger in genetically predisposed individuals.
When one is stressed, the adrenal gland releases cortisol (the stress hormone) into the body, increasing the level of dopamine in the brain; this change can be linked to the development of a mental illness, such as a shared delusional disorder.
Type of delusions
Delusions are fixed, unshakeable and persistent beliefs or misconceptions, thus not changing even when a person is presented with conflicting evidence.
A delusion, in order to be considered as such, must be considered in the historical-social-cultural environment of the subject: for example, some ideas of an Australian aborigine or an ancient Roman or a Spaniard who lived in the Middle Ages, should not be considered delusions even though they may be considered as such by an Italian living in the year 2000.
The delusions that can affect individuals affected by madness in twos can be of various types.
Bizarre delusions
These are those that are clearly implausible and not understood by peers within the same culture, even those with psychological disorders; for example, an individual may think that all their organs have been removed and replaced by someone else’s while they slept without leaving scars and without waking up.
Or an individual may think that he or she is already dead.
Or the patient is convinced that one’s thoughts or emotions are under the control of some external force or that one’s ideas have been replaced with those of other people.
Non-bizarre delusions
Common among those with personality disorders and understood by people within the same culture.
For example, unfounded or unverifiable claims of ‘conspiracies’ such as being followed by the FBI in unmarked cars and observed by security cameras are classified as non-bizarre delusions.
Delusions congruent with mood
These correspond to a person’s emotions within a certain period of time, especially during an episode of mania or depression.
For example, a person with mania and this type of delusion may believe with certainty that he or she will win a million euros at roulette on a specific night, despite obviously having no way of predicting the future or influencing the probability of such an event.
Similarly, someone in a depressive state may feel certain that their mother will be struck by lightning and die the next day, despite having no means of predicting or controlling future events.
Neutral mood delusions
In contrast to mood congruent delusions, neutral mood delusions are not affected by mood and may be bizarre or non-bizarre; the formal definition provided by Mental Health Daily is ‘a false belief that is not directly related to the person’s emotional state’.
Biopsychosocial consequences of shared psychotic disorder
As with many psychiatric disorders, shared delusional disorder can have a strongly negative impact on the psychological and social aspects of a person’s well-being.
The unresolved stress resulting from a delusional disorder will eventually contribute to or increase the risk of other negative health outcomes, such as cardiovascular disease, diabetes, obesity, immunological problems, and other illnesses.
These health risks increase with the severity of the illness, especially if an affected person does not receive or adhere to appropriate treatment.
People with a delusional disorder have a significantly high risk of developing psychiatric comorbidities such as depression and anxiety.
Shared delusional disorder can have a profoundly negative impact on a person’s quality of life
People diagnosed with a mental health disorder commonly experience social isolation, which can lead to violent acts against themselves (self-mutilation, suicide…) and others.
An individual with shared delusional disorder tends not to be able to manage their job and be fired, and not to be able to manage a marriage and possible children (loss of parental authority and divorce).
Shared delusional disorder is often difficult to diagnose
Usually, the person with the condition does not seek treatment, as they do not realise that their delusion is abnormal because it comes from someone in a dominant position whom they trust.
Moreover, as their delusion gradually manifests itself and strengthens over time, their doubt slowly weakens during this period.
Shared delusional disorder is diagnosed when the patient meets three criteria:
- the patient must have a delirium that develops in the context of a close relationship with an individual with an already established delirium;
- the delirium must be very similar or even identical to that established by the other individual with delirium;
- the delirium cannot be better explained by any other psychological disorder, mood disorder with psychological features, a direct result of the physiological effects of substance abuse or any general medical condition.
Shared psychotic disorder in DSM-4, ICD-10, DSM-5
The psychiatric classifications contained in the penultimate version of the Diagnostic and Statistical Manual of Mental Disorders and the latest version of the International Classification of Diseases refer to Lasègue-Falret syndrome as shared psychotic disorder (DSM-4 – 297.3) and induced delusional disorder (ICD-10 – F24), although the medical literature largely uses the original name.
However, this disorder is not present in the latest version of the DSM (the DSM-5, published in the USA in May 2013 and in 2014 in Italy), which considers the criteria insufficient or inadequate. The DSM-5 does not consider Lasègue-Falret syndrome as a separate entity, but as ‘delusional disorder’ or ‘other specified schizophrenic spectrum’ and ‘other psychotic disorder’.
Treatment of shared psychotic disorder
The first step in treatment is to separate the two persons: generally, in two-set insanity, this may be enough to make the delusions transmitted by the inducer disappear or diminish over time.
If this is not enough to stop the delusions, there are two possible courses of action: pharmacological and non-pharmacological.
With treatment, the delusions, and thus the illness, will eventually diminish so much that it will practically disappear in most cases.
However, if left untreated, it can become chronic and lead to anxiety, depression, aggressive behaviour and further social isolation: in such cases, the delusions will probably not disappear even if the two are separated.
Drug therapy
If separation alone does not work, antipsychotic drugs are often prescribed for a short period to prevent the delusions.
Antipsychotics are drugs that reduce or alleviate the symptoms of psychosis such as delusions or hallucinations.
Other uses of antipsychotics include stabilising mood for people with mood swings and mood disorders (i.e. in bipolar patients), reducing anxiety in anxiety disorders and reducing tics in people with Tourettes.
Antipsychotics do not cure psychosis, but help reduce symptoms. Medications are more successful if they are combined with non-drug therapy.
Although antipsychotics are powerful and often effective, they have side effects, such as the induction of involuntary movements, so they should only be taken if absolutely necessary and under the supervision of a psychiatrist.
Non-pharmacological therapy
The two most common forms of therapy for persons with shared delusional disorder are personal therapy and family therapy:
- Personal therapy is individual counselling that focuses on building a relationship between the counsellor and the patient and aims to create a positive environment in which the patient feels they can speak freely and truthfully. This is advantageous, as the counsellor can usually get more information from the patient to get a better idea of how to help him/her. Furthermore, if the patient trusts what the counsellor says, it will be easier to disprove the illusion.
- Family therapy is a technique in which the whole family enters therapy together to work on their relationships and to find ways to eliminate the illusion within the family dynamic. For example, if someone’s sister is the inducer, the family will need to be involved to ensure that the two are separated and to understand how the family dynamic will work around this. The more support a patient has, the more likely they are to recover, especially since insanity in twos usually occurs due to social isolation.
Prognosis
Unfortunately, there are not many statistics on the prognosis of shared delusional disorder, as it is a very rare disease and it is thought that most cases go unreported; however, with proper treatment, the prognosis is usually very good.
Controversies
Admitting that the delusional ideas of a group of people suffering from such a disorder are indeed delusions would, however, conflict with a tenet of psychiatry: the Diagnostic and Statistical Manual of Mental Disorders states that a person CANNOT be diagnosed as delusional if the belief in question is commonly accepted by other members of their culture or subculture (otherwise even the Catholic religion, with its belief in an invisible god would be considered psychiatrically relevant).
When a fairly large community of people therefore ends up believing something false – or at least NOT demonstrable – and potentially dangerous based solely on ‘hearsay’, these beliefs are therefore not considered ‘delusions’, but rather ‘mass hysteria’.
A world-wide religion is, in some ways, a set of delusions so widespread that it gives rise to a mass hysteria that has in turn become so widespread that it has become ‘normal’.
When an ‘official’ religion ceases to be widespread, it becomes delusional again: for example, believing in the idea of the existence of Zeus today is considered delusional, but psychiatry would not have considered it so 2000 years ago. Religion becomes delirium again when it ceases to be widespread.
Curiosity
The film by director Todd Phillips, starring Joaquin Phoenix and Lady Gaga, which will be released in cinemas in October 2024 as a sequel to the film Joker (2019), will be called “Joker: Folie à deux”.
It is assumed, therefore, that there are references in the plot to the very psychiatric illness discussed in this article.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What You Need To Know About Substance Use Disorder
Schizophrenia: Risks, Genetic Factors, Diagnosis And Treatment
Obsessive-Compulsive Personality Disorder: Psychotherapy, Medication
Seasonal Depression Can Happen In Spring: Here’s Why And How To Cope
Intranasal Ketamine For The Treatment Of Patients With Acute Pain In ED
Delirium And Dementia: What Are The Differences?
The Use Of Ketamine In Pre-Hospital Setting – VIDEO
Anxiety: A Feeling Of Nervousness, Worry Or Restlessness
What Is OCD (Obsessive Compulsive Disorder)?
Ketamine May Be Emergency Deterrent For People At Risk Of Suicide
Everything You Need To Know About Bipolar Disorder
Drugs To Treat Bipolar Disorder
What Triggers Bipolar Disorder? What Are The Causes And What Are The Symptoms?
Antipsychotic Drugs: An Overview, Indications For Use



