What is angioplasty?
Angioplasty is a procedure that creates more space inside an artery that has plaque built up inside it. Your healthcare provider uses a tiny balloon to force plaque against the artery walls so blood can get through your artery
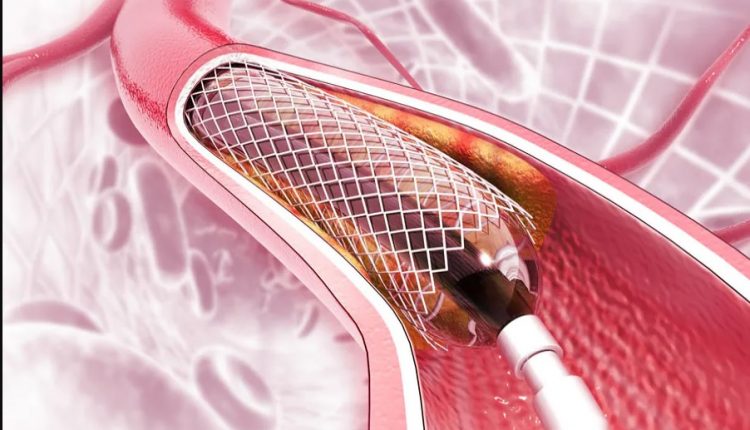
Often, they also place a stent or tube inside the newly opened space to keep it open
Angioplasty, also called balloon angioplasty, is a procedure that opens arteries to let blood go through more easily.
Healthcare providers use this minimally invasive procedure in tight spots in arteries where plaque makes the space inside an artery too narrow or blocks it.
Who needs to have angioplasty?
People who have coronary artery disease or a heart attack may need to have coronary angioplasty.
Angioplasty is also used in other parts of the body that have narrow or blocked arteries, such as your neck, arms and legs, kidneys and pelvis.
Angioplasty allows more blood to get through an artery that’s too narrow or blocked with plaque.
This means the organ that artery reaches will get a better supply of blood after angioplasty.
What does angioplasty treat?
- Angioplasty treats atherosclerosis (a collection of plaque made of fat and cholesterol) in your arteries in several different places in your body.
- Coronary artery disease. Coronary angioplasty, or percutaneous coronary intervention, can help you if you have a narrow or blocked coronary artery that’s keeping your heart from getting the oxygen it needs, causing chest pain and/or a heart attack.
- Peripheral artery disease. Angioplasty treats atherosclerosis in the major arteries in your arms, legs and pelvis.
- Carotid artery disease. Angioplasty can help with blocked arteries in your neck. Left untreated, they can lead to a stroke if your brain isn’t getting enough oxygen.
- Chronic kidney disease. When plaque collects in the arteries in your kidneys, it affects how much oxygen can reach your kidneys. Sometimes a renal artery angioplasty can help.
How common is angioplasty?
Coronary angioplasty is one of America’s most common procedures.
What happens before angioplasty?
Your provider will usually ask you to stop drinking or eating for a few hours before your angioplasty procedure.
You can plan on your angioplasty procedure taking a half-hour to a few hours, depending on your situation.
At the hospital, you’ll put on a hospital gown.
You’ll need to tell your provider what medicines you take and what allergies you have.
Your healthcare provider will put an IV in your arm to give you medicine that will relax you.
You’ll still be able to respond to your provider’s questions.
You’ll also get medicine in your IV that will keep your body from making blood clots.
What happens during angioplasty?
This description will be about a coronary angioplasty, but providers perform angioplasty in a similar way on other parts of your body.
However, they may put the catheter in through a different artery than they would for the heart.
Your provider puts a catheter or tube through your skin and into a blood vessel in your wrist or groin.
They use medicine to keep you from feeling the tube go into your body.
With X-rays to help find the way, a cardiologist, or heart expert, moves the catheter (tube) through your blood vessels to get to your blocked or narrowed coronary artery.
You might feel warm briefly when they release a dye through the catheter to make it easier to see your blood vessels.
When they get to the problem area, your provider will put in a wire and another catheter (a balloon catheter) that has a very small balloon at the end of it.
Once they inflate the balloon, it moves the plaque out of the way and off to the side of the artery wall. This clears the way for blood to get through.
Your narrow coronary artery is like a crowded subway car with people blocking the aisle.
In order for people to get through the aisle, others need to move closer to the walls.
The catheter balloon is like a football team that would force everyone to the side of the subway car so they could get through the aisle.
Your provider will usually then put in a stent, a small hollow scaffold made of metal.
Stronger than a balloon, the stent keeps the artery open after balloon removal.
The stent, which your provider expands and locks into position after it’s put in your artery, stays inside your artery long after the angioplasty is done.
Many stents have a drug coating that helps prevent your artery from getting too narrow again.
If you have peripheral artery disease, your provider may use a balloon that transfers its medicine coating to the artery wall.
The drug stays behind after the balloon is taken out.
You may feel some discomfort when your provider inflates the balloon, but that goes away when they deflate it.
Your healthcare provider deflates the balloon after it has done its job.
The balloon can be inflated a couple of times in the same spot or in another blocked artery in your body.
Using an angiogram (X-ray images of your blood vessels), your provider can compare how well your blood flowed before and after your angioplasty to see how well it worked.
What happens after angioplasty?
Your provider will take out the catheters and use a bandage to cover the place where the catheters went into your skin.
You may feel someone pressing on the wound to stop the bleeding.
You might be sore or have a bruise there later.
What are the advantages of angioplasty?
Benefits of angioplasty include:
- It has less risk and a lower cost than a surgical procedure.
- You’ll only have one wound from where the catheters were and a smaller wound from your IV.
- Your provider can put in a stent during your angioplasty if you need it.
What are the risks or complications of angioplasty?
It’s rare to have serious complications after an angioplasty, but every invasive procedure comes with occasional risks.
For example, you may need an emergency coronary artery bypass graft during or soon after an angioplasty.
Complications happen in around one in 100 procedures, although this might be higher or lower depending on your individual circumstances.
Other angioplasty risks include:
- A reaction to the dye.
- Heart attack.
- Abnormal heart rhythm.
- Stroke.
- Blood vessel or kidney damage.
- Blood clots.
- Chest pain.
- Bleeding.
A repeat blockage if a stent isn’t placed in your artery.
The risk of angioplasty complications is higher for older adults or people who have several blocked arteries, kidney disease or heart failure.
What is the recovery time after angioplasty?
You’ll need to stay at the hospital for several hours or even overnight to recover from angioplasty.
Your healthcare provider will tell you what medicines you need and how active you can be after your angioplasty.
You’ll need to have someone drive you home from the hospital because you had anesthesia.
Get rest at home and drink fluids.
Don’t exert yourself for the next 24 hours.
You may need to take medicines like aspirin or other blood thinners after your angioplasty procedure.
If your healthcare provider prescribed blood thinners, it’s important to take these as directed.
Do not miss any doses.
If you think you need to stop taking blood thinners, you should discuss it with your provider before you do.
When can I go back to work or drive?
You should be able to drive and go back to work about a week after your coronary angioplasty.
The time may be shorter for other types of angioplasty.
Check with your provider.
When should I see my healthcare provider?
You’ll have a follow-up visit after you go home, but you should contact your provider if:
- You have bleeding or an infection where the catheters went through your skin.
- Your leg color changes.
It hurts or feels warm where the catheters were.
You should also tell your provider if you’re having trouble with the anticlotting medicine you take for three to 12 months after receiving a stent.
Angioplasty can make a difference in how well your blood flows through an artery that had a collection of plaque in it.
But even after a successful angioplasty and stent placement, it’s important to live a healthy lifestyle.
This includes eating a healthy diet, exercising and not using tobacco products.
Be sure to keep taking medicines your provider prescribed and go to all of your follow-up appointments.
References
- National Heart, Lung, and Blood Institute. Percutaneous Coronary Intervention. (https://www.nhlbi.nih.gov/health-topics/percutaneous-coronary-intervention) Accessed 11/2/2021.
- NHS. Recovery: Coronary angioplasty and stent insertion. (https://www.nhs.uk/conditions/coronary-angioplasty/recovery/) Accessed 11/2/2021.
- Radiological Society of North America Inc. Angioplasty and Vascular Stenting. (https://www.radiologyinfo.org/en/info/angioplasty) Accessed 11/2/2021.
- StatPearls. Percutaneous Transluminal Coronary Angioplasty. (https://www.ncbi.nlm.nih.gov/books/NBK535417/) StatPearls Publishing. 2021 Jan. Accessed 11/2/2021.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Carotid Angioplasty And Stenting: What Are We Talking About?
Percutaneous Transluminal Coronary Angioplasty (PTCA): What Is It?
Aneurysm Surgery: Traditional Open Surgery
Atrial Fibrillation: Symptoms To Watch Out For
Coronary Angioplasty, What To Do Post-Operatively?
Heart Patients And Heat: Cardiologist’s Advice For A Safe Summer
US EMS Rescuers To Be Assisted By Paediatricians Through Virtual Reality (VR)
Coronary Angioplasty, How Is The Procedure Performed?
Atrial Fibrillation: Causes, Symptoms And Treatment
Cardiac Rhythm Disturbance Emergencies: The Experience Of US Rescuers
Prenatal Pathologies, Congenital Heart Defects: Pulmonary Atresia
Management Of Cardiac Arrest Emergencies
Palpitations: What Causes Them And What To Do
The J-Curve Theory In High Blood Pressure: A Really Dangerous Curve
Why Children Should Learn CPR: Cardiopulmonary Resuscitation At School Age
What Is The Difference Between Adult And Infant CPR
Long QT Syndrome: Causes, Diagnosis, Values, Treatment, Medication
What Is Takotsubo Cardiomyopathy (Broken Heart Syndrome)?
The Patient’s ECG: How To Read An Electrocardiogram In A Simple Way
Stress Exercise Test Inducing Ventricular Arrhythmias In LQT Interval Individuals
CPR And Neonatology: Cardiopulmonary Resuscitation In The Newborn
First Aid: How To Treat A Choking Baby
How Healthcare Providers Define Whether You’re Really Unconscious
Concussion: What It Is, What To Do, Consequences, Recovery Time
AMBU: The Impact Of Mechanical Ventilation On The Effectiveness Of CPR
Defibrillator: What It Is, How It Works, Price, Voltage, Manual And External
The Patient’s ECG: How To Read An Electrocardiogram In A Simple Way
Emergency, The ZOLL Tour Kicks Off. First Stop, Intervol: Volunteer Gabriele Tells Us About It
Proper Defibrillator Maintenance To Ensure Maximum Efficiency
First Aid: The Causes And Treatment Of Confusion
Know What To Do In Case Of Choking With Child Or Adult
Choking Children: What To Do In 5-6 Minutes?
What Is Choking? Causes, Treatment, And Prevention
Respiratory Disobstruction Manoeuvres – Anti-Suffocation In Infants
Resuscitation Manoeuvres: Cardiac Massage On Children
The 5 Basic Steps Of CPR: How To Perform Resuscitation On Adults, Children And Infants



